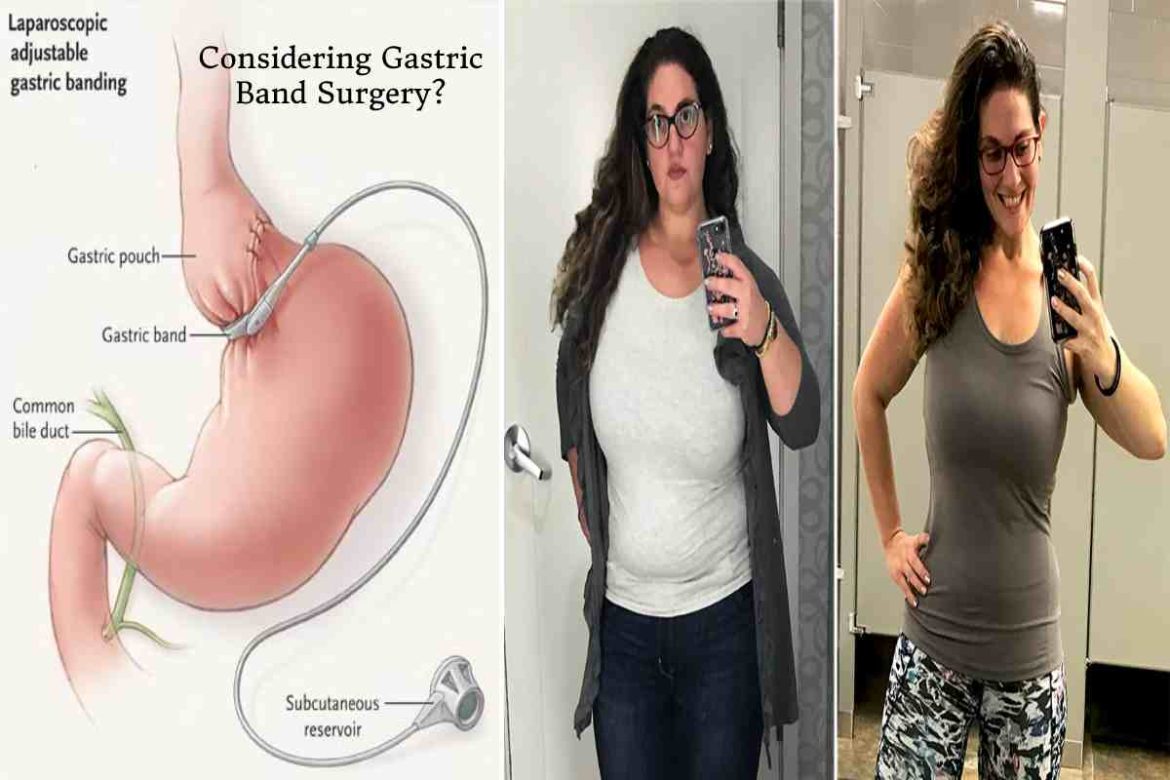
Considering Gastric Band Surgery? – Gastric band surgery is an adjustable, reversible, quick, and minimally invasive weight loss surgery that constricts the stomach. This, in turn, reduces the amount of food you need to eat to feel full. The procedure involves placing a band around the stomach’s top, which helps you feel full and satiated with less food.
After surgery, you need to follow a liquid-only diet for up to 6 weeks while slowly reintroducing soft foods into your diet.
The procedure is used to treat severely obese people who aren’t able to lose weight with just exercise and diet. It improves diabetes and can ensure dramatic weight loss. It is also FDA-approved.
So if you’re thinking of getting private gastric band surgery, here’s everything you need to know.
How does it work?
In gastric band surgery, a silicone band is placed around the top of the stomach to reduce its size. This, in turn, lowers the food intake. Adjusting the band changes how much the stomach is constricted.
A tube is attached to the band and is accessible via a port under the abdomen’s skin. The surgeon uses this port to inject a saline solution, which inflates the band and divides the stomach into two: a small pouch with an inch-wide outlet on top and the remainder of the abdomen below.
The food you eat during a meal goes into the small pouch. It then slowly makes its way into the lower part of the stomach and is gradually digested. In the first few weeks after the surgery, the small pouch can only hold up to an ounce of food. Over time, it can hold up to 2-3 ounces. This results in you feeling full and satiated after only a small serving.
All in all, gastric band surgery works by reducing hunger, which ultimately lowers your overall food intake. Unlike other bariatric procedures, gastric band surgery doesn’t cause malabsorption.
The procedure
Once you decide to go ahead with gastric band surgery, the surgeon will fit the gastric band while you’re under general anaesthesia. The procedure is usually carried out in an outpatient clinic, and if all goes well, you don’t need to spend a night in the hospital.
Gastric band surgery is minimally invasive and is performed via keyhole incisions. Your surgeon will make 1-5 small surgical cuts in your abdomen and use a laparoscope (a camera attached to a long, narrow tube). The surgery can take anywhere from 30 minutes to 60 minutes.
If you’re getting the surgery, make sure you don’t eat anything the day of your surgery. You will be able to go about with your daily activities two days after the surgery, but you might have to rest for a week and not do anything strenuous.
Who qualifies for gastric band surgery?
If you do your own research, you will find guidelines stating that you can only get gastric band surgery if your BMI is over 35. Or if you have any obesity-related problem like sleep apnea, hypertension, or diabetes, then your BMI should be above 30 because of the risk of complications involved. But this was in the past; advancements in surgical techniques have made the process safer, and these guidelines no longer hold true.
Your doctor may recommend you get a gastric band surgery if you have obesity-related complications or if non-surgical approaches like exercise, dietary changes, and medications don’t have the desired effects.
However, gastric band surgery is not for you if you have an alcohol or drug use disorder or are unwilling to make the lifestyle changes you will have to make after the surgery.
Benefits of gastric band surgery
A gastric band surgery provides the following benefits:
- Long-term weight loss results, especially for obese people. On average, people lose 40-60% of the extra weight, but the results vary from person to person
- It doesn’t lead to malnutrition, unlike other weight-loss surgeries
- Reduces risk of conditions related to high weight, including urinary incontinence, high blood pressure, and diabetes
- Short recovery time compared to other surgery options
- Lesser chances of hernias and wound infections after surgery
- Improved quality of life
- Irreversible procedure; you can get the band taken out
- The band can be loosened or tightened if you tend to vomit after eating or if you think you haven’t lost enough weight
Risks & complications
Some risks and complications associated with this bariatric surgery option include:
- You might have an adverse reaction to the anaesthesia, including infection, allergic reaction, blood loss, blood clots in the lungs, and breathing problems. In some cases, you might experience a stroke or heart attack during or even after the surgery.
- While the procedure guarantees lasting results, the weight loss is slower than other weight-loss surgeries.
- The silicone band can have mechanical problems and may require another doctor’s visit. It can also slip or erode, in which case it will need to be removed.
- The oesophagus and stomach can be stretched, causing you to regain weight.
- The port attached to the tube can also shift. If this happens, you will need another surgery. Up to 60% of people report needing a follow-up surgery.
- You need to strictly follow the dietary recommendations since overeating can cause vomiting and oesophagus dilation.
- You might have trouble swallowing or experience nausea after the surgery.
- Saline can leak from the band.
In addition, like with all other weight loss surgery options, gastric band surgery poses the following risks:
- Injury to the intestines, stomach, and other abdominal organs
- Stomach ulcers, heartburn, and inflamed stomach lining
- Lack of nutrition because of the reduced food intake
- Gastrointestinal scarring and bowel blockage
Conclusion
Gastric band surgery is a major change and requires you to change your lifestyle and diet, too. Make sure you understand all the risks and complications of the surgery before going ahead with it. Also, make sure you discuss the procedure with your healthcare provider first to be absolutely sure of your decision.